Blood cultures in the Pediatric Service of the “Dr. Juan Tanca Marengo”, National Oncology Institute of Solca-Guayaquil.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Luis Espín Custodio, Anibal Bonilla Nuñez, Jessica Valeria Andrade Rada

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
DOI:
https://doi.org/10.33821/87Keywords:
BLOOD CULTURE, PEDIATRIC HOSPITALS, NEUTROPENIA, PEDIATRIC, MULTI-RESISTANT BACTERIA, BACTERIAL INFECTIONS AND MICOSIS, GRAMNEGATIVE BACTERIA, GRAMPOSITIVE BACTERIAAbstract
Introduction: The increasing antibiotic resistance of isolated microorganisms in blood cultures in neutropenic patients makes it necessary to continuously monitor the antibiogram to monitor the changing antibiotic susceptibility. The objective of this study was to identify during one year the isolated microorganisms of blood cultures and their sensitivity, in children with cancer admitted to an Oncological Institute.
Methods: This is a prospective study of data collected from June 2017 to June 2018, with isolation of blood cultures in febrile neutropenic patients hospitalized in the pediatric area of ??the National Oncology Institute “Dr. Juan Tanca Marengo ”Solca, Guayaquil.
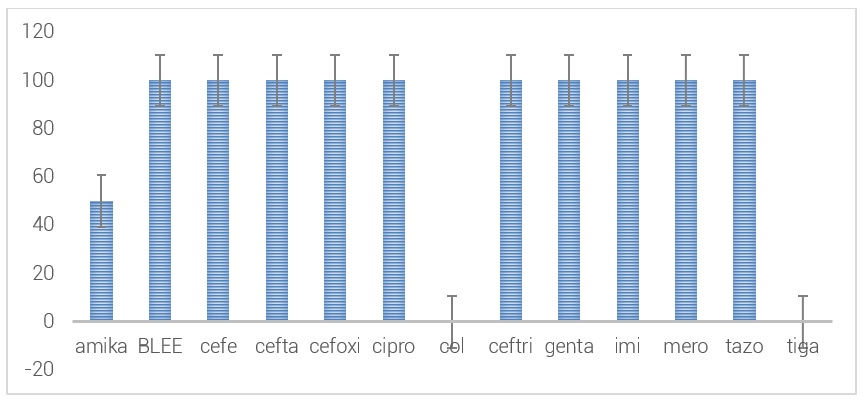
Results: There were 183 patients, 133 (72%) with hematological malignancies and 50 (28%) with solid tumors. In this group 265 blood cultures were taken. 100 reports (38%) were positive, 66% were Gram-Positive bacteria and 34% Gram-negative. The most frequent bacteria 20% E. epidermidis, 18% E. aureus, 17% E. haemolyticus, 12% E. Coli, 10% Staphylococcus hominis, 9% Klebsiella Pneumoniae, 6% Pseudomona species, 5% Acinetobacter, Gram bacteria -positives were 100% sensitive to linezolid, vancomycin and tigacillin; while Gram-negatives maintain a sensitivity of 91% to amikacin, 59% to cefepime, 59% to ceftazidime, 77% to ciprofloxacin, 68% to imipenem, 76% to meropenem, 56% to piperacillin-tazobactam, 100% at colistin and 97% at tigecycline. An increase in multi-resistant Carbapenemase-producing Klebsiella Pneumoniae (KPC) was observed, 100% sensitive to tigacycline and colistin and 50% to amikacin.
Conclusion: The incidence was higher for gram-positive bacteria. There is a good sensitivity to vancomycin, linezolid and tigacycline for gram-positive bacteria; and to amikacin, colistin and tigacillin for Gram-negatives. The multi-resistant KPC bacteria were only sensitive to tigecycline and colistin.