Clinical Case: Autoimmune Cytopenia as an immunological complication of Allogeneic Unrelated Donor Transplantation, in a pediatric patient with Sickle Cell Anemia.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Migleth Cisneros López, Bella Maldonado Guerrero, Aníbal Bonilla Núñez, Andrés Gonzalez Cabrera, Jessica Andrade Rada

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
DOI:
https://doi.org/10.33821/462Keywords:
LEUKOPENIA, THROMBOCYTOPENIA, PERIPHERAL BLOOD STEM CELL TRANSPLANTATION, AUTOIMMUNE DISEASESAbstract
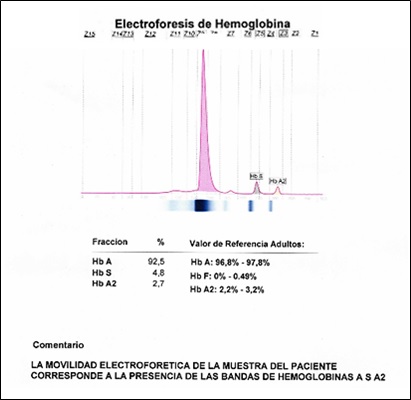
Introduction: Sickle cell disease is an inherited condition in which an abnormal hemoglobin is produced that impairs tissue oxygenation, vaso-occlusive crises and hemolytic reactions. Patients with this disease present an abnormal activation of the complement pathway, leading to an increase in the frequency of infections and autoimmune diseases. We present a case of association of an autoimmune disease in a patient with sickle cell disease.
Clinical case: 10-year-old boy with sickle cell anemia (2009) with splenectomy and recurrent veno-occlusive crisis, underwent Allogeneic transplantation in April 2019 outside the institution with an unrelated isogroup O + donor (10/10). Treated with: Fludarabine - Busulfan, Thymoglobulin + and Metotexate. He developed autoimmune bicytopenia and febrile syndrome at +165 day post HSCT. White blood cells: 360 uL, neutrophils: 14%, hemoglobin: 7.90 g / dL, platelets: 25,000 uL, ferritin: 4695 ng / ml, total IgG: 9.88 gr / l, LDH: 190 IU / l. C-reactive protein: 2.79 mg / dL, procalcitonin 0.13 ng / mL.
Evolution: after ruling out viral infection, the patient completed a broad-spectrum antibiotic treatment and underwent suspension of immunosuppressive treatment due to suspected toxicity, with no response. A medullary study by flow cytometry was performed, determining a decrease in the B lymphoid line, and autoimmune cytopenia was concluded as an immunological complication of the transplant.
Outcome: The patient received transfusion therapy (plateletpheresis + concentrated red blood cells). He also received IV methylprednisolone for 3 days and 30 mg prednisone for 14 days with gradual subsequent reduction to start Rituximab and cyclosporine. The treatment with Immunoglobulin 6g IV for 5 days was completed. At discharge, white blood cells: 5080 uL, neutrophils: 67%, hemoglobin: 9.20 g / dL, platelets: 20,000 uL, after 18 days of hospital admission.
Conclusion: The results with treatment in this case suggest that it may be reasonable to consider autoimmune cytopenias as a diagnostic hematological manifestation of chronic GVHD. Alternatively, it is possible to treat immune cytopenia with steroids, rituximab, and other immunosuppressants.