Observational Study: Use of Antimicrobials in the Intensive Care Unit of the SOLCA-Guayaquil Hospital.
Publications of the Project "ANTIMICROBIAL STEWARDSHIP" in Latin America (PROA).
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Carlos Enrique García Cruz, Janeth Alexandra Zambrano Meza, José Mauricio Fajardo Herrera, Aquiles Eduardo Bowen Flores

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
DOI:
https://doi.org/10.33821/450Keywords:
CROSS INFECTION, BETA-LACTAM RESISTANCE, INTENSIVE CARE UNITS, ANTIMICROBIAL STEWARDSHIPAbstract
Introduction: Antimicrobial use optimization programs (PROA) arise due to the need to decrease the percentage of infections by antimicrobial resistant microorganisms, which would benefit from better clinical results, reducing adverse effects and reducing the expense involved in the use of the same. This program was implemented in the intensive care unit of the SOLCA Guayaquil cancer hospital for one year. The objective of the present study was to establish the rate of use of antimicrobials in an Intensive Care Unit (ICU), the percentage of descaling and the epidemiology of infections in the ICU.
Methods: In this prospective observational study, with a non-probability sample, all the cases admitted to the ICU of the Dr. Juan Tanca Marengo National Oncological Institute in the city of Guayaquil, in the period July 2018 to June 2019 were included. The variables were prevalence of the antibiotic use, type of antibiotic used, antibiotics displacement, staff adherence to clinical guidelines and defined daily doses (DDD) and the patient-day-month index by hospitalization area.
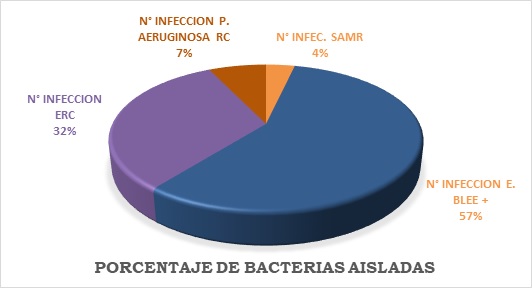
Results: 246 patients were included; 81% were receiving antibiotics, with a maximum of two antibiotics per patient; Surgical prophylaxis was maintained within the first 24 hours 50% of the time and 25.66% received it for a period greater than 24 hours; 57.25% had a sustained offset, in 20.75% the scaled type and 13.66% the bare type. Isolated pathogens include 57% positive extended spectrum beta lactamase-producing enterobacteriaceae (ESBL +) and 32% carbapenem-resistant enterobacteriaceae. The highest consumption was of carbapenems with 625.24 g. followed by beta-lactamase inhibitors with 402.94 g. The empirical treatment rate of 49.58% vs. 26.41% of targeted treatments; and gross mortality of 22.76%.
Conclusion: The rate of use of antibiotics in the ICU is high, the percentage of descaling was acceptable compared to the rates reported regionally, the epidemiology of the most frequent reported germs are the extended spectrum beta lactamase-producing enterobacteriaceae.