Non-beneficial Interventions in Palliative Patients Treated at Intensive Care Units
in South America: A Systematic Review
Article / Artículo
https://doi.org/10.33821/815
Date received: 19/8/2025
Date accepted: 20/11/2025
Introduction
In recent decades, technological advances in critical care medicine have made it possible
to prolong the lives of patients whose prognoses were previously considered incompatible
with survival. However, these advances have also raised complex ethical dilemmas,
especially concerning medical interventions that, in the context of advanced or terminal
illness, may be seen as futile or disproportionate. These practices, known as non-beneficial
therapeutic interventions, do not offer significant improvement in the patient's prognosis
or quality of life, which creates conflicts with the principles of autonomy, beneficence,
non-maleficence, and justice [1].
In this context, palliative care emerges as an ethical, humanistic, and scientific
response. According to the World Health Organization, this approach aims at alleviating
suffering and improving the quality of life for patients with incurable or terminal
illnesses, as well as for their families [2]. However, in intensive care units (ICUs) in South America, there is a constant tension
between using all available technological resources and the need to ensure the principles
of therapeutic proportionality and human dignity, which generates ethical dilemmas
and challenges in care practices [3,4].
Despite its international recognition as an essential component of healthcare, the
integration of palliative care in South American ICUs continues to be limited and
uneven. Recent reports from the Pan American Health Organization and various regional
studies show that institutional, cultural, and educational factors hinder the adoption
of practices that prioritize the integral well-being of patients at the end of life
[5-9]. Additionally, healthcare professionals face clinical uncertainty, family pressures,
fear of litigation, and a prevailing curative approach, all of which limit the implementation
of shared and ethically justified decisions in critical contexts [10-12].
Evidence indicates that training in clinical ethics and the application of strategies
such as limitation of therapeutic effort (LTE) are fundamental tools to prevent therapeutic
obstinacy in critical care contexts [13,14]. Nevertheless, a better understanding of how these strategies are implemented in
everyday practice is still needed, especially in public hospitals and among oncology
patients or those with poor vital prognosis, where ethical decisions tend to be more
complex and are influenced by structural and cultural limitations.
In light of this issue, the present study is justified by the need to understand and
reflect upon non-beneficial therapeutic interventions in palliative patients treated
at ICUs in South America. These practices not only undermine the quality of care but
also conflict with fundamental principles of bioethics and the recognition of palliative
care as a human right [15]. Similarly, the limited incorporation of palliative care in critical care settings
in the region reflects a knowledge and action gap that, according to international
recommendations, should be addressed through implementation guidelines adapted to
the local context [16].
Furthermore, it is essential to promote patient- and family-centered care processes
based on care ethics and bioethical reflection that integrate interdisciplinary support
and respect for human dignity [17,18]. Training healthcare professionals in palliative care is key to ensuring clinical
decisions grounded in evidence and in the patient’s values [19]. In this regard, tools such as limitation of therapeutic effort (LTE) and do-not-resuscitate
orders have been identified as ethically necessary resources to address end-of-life
dilemmas [20].
This review aims at analyzing recent scientific literature on the approach to palliative
care and non-beneficial therapeutic interventions at intensive care units in South
America, identifying factors that contribute to the persistence of such interventions
in palliative patients, exploring the degree of integration of palliative care into
ICUs and its relationship with clinical decision-making, and examining the ethical
and clinical competencies of healthcare professionals when facing end-of-life situations
in critical care settings.
Methodology
A literature review with a qualitative approach was conducted.
2.1 Search strategy and study selection
The literature search was carried out in the PubMed, SciELO, Redalyc, Dialnet, and
Google Scholar databases. The search strategy focused on combining the DeCS/MeSH descriptors
“palliative care,” “intensive care units,” “appropriateness of therapeutic effort,”
“non-beneficial therapeutic interventions,” and “South America,” using the Boolean
operators “AND” and “OR.”
2.2 Inclusion criteria
-
Peer-reviewed scientific articles published in the last five years.
-
Original articles and articles relevant to the objective of the research.
-
Literature in Spanish and English.
2.3 Exclusion criteria
-
Theses, non-peer-reviewed works, or essays without a clear methodology.
-
Articles focused on home or out-of-hospital palliative care.
-
Publications prior to 2021.
2.4 Selection process
Initially, 94 potentially relevant articles were identified. After applying the inclusion
and exclusion criteria, 30 articles that met the required thematic relevance were
selected and are shown in a PRISMA flow diagram.
2.5 Methodological quality assessment instruments
To ensure the transparency and rigor of the review, the following instruments were
applied:
-
Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ)
checklist: compliance with 18 out of 21 items.
-
PRISMA 2020 checklist: compliance with 26 out of 27 items. No registration was performed
in the International Prospective Register of Systematic Reviews (PROSPERO).
-
Critical Appraisal Skills Programme (CASP): the ten criteria for qualitative studies
were applied, it must comply with nine of them. The main limitation was the scarce
explicit reflexivity of the researchers in some studies.
2.6 Analysis procedures
Studies underwent an individual critical appraisal using the qualitative version of
CASP, taking into consideration design, data collection methods, clarity in presenting
results, clinical implications, and methodological rigor.
These tools and procedures ensured the reproducibility, transparency, and methodological
validity of this study. They also provided a solid foundation for analysis and formulation
of clinical and ethical recommendations.
3. Results
Initially, 94 records were identified in the SciELO, Redalyc, PubMed, Dialnet, and
Google Scholar databases. After removing 16 duplicates, 78 titles and abstracts were
reviewed. Out of those, 40 were considered potentially relevant for full-text reading.
Finally, 30 studies met the inclusion criteria and were incorporated into the qualitative
synthesis of the review (Figure 1).
Figure 1
Flow diagram of article selection according to the PRISMA model.
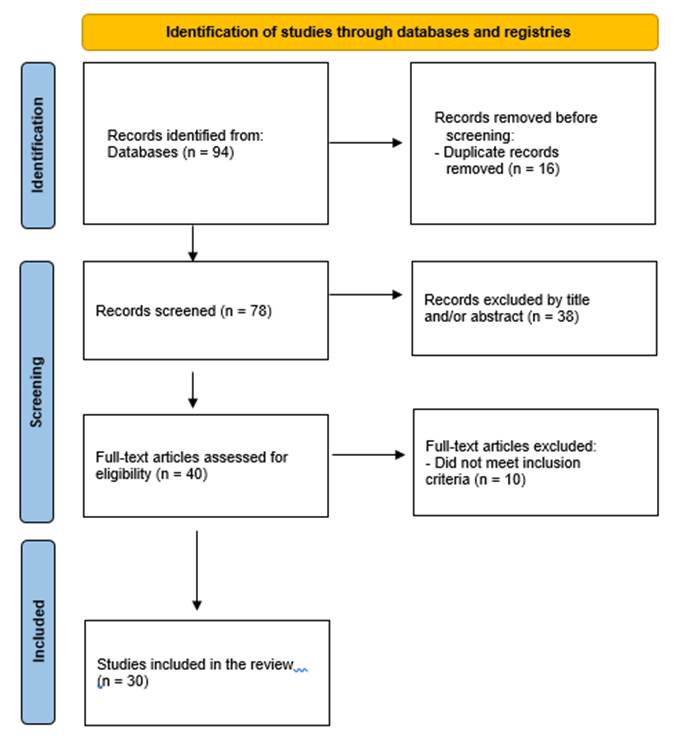
Source: Own elaboration based on the PRISMA 2020 flowchart.
Findings were organized around the three specific objectives defined in the review,
as detailed below.
3.1. Factors favoring the persistence of non-beneficial interventions in the ICU
Findings confirm that the persistence of non-beneficial interventions in critically
ill patients is linked to multiple structural, cultural, and legal factors. Among
the most significant are the absence of institutional protocols, family pressure,
and fear of legal repercussions. These lead to the prolongation of life with invasive
treatments in situations where recovery is not possible [1, 3, 4, 6, 7, 11-14, 21].
Additionally, other studies have highlighted the impact of the digitalization of medicine
and the increasing technification of critical care, where dependence on medical devices
reinforces the practice of therapeutic obstinacy [22]. Recent research also shows that the biomedical culture in Latin America, which
is strongly cure-oriented, makes it difficult to recognize therapeutic futility and
limits the development of ethical deliberation spaces [23-25].
The humanization of care, understood as a fundamental axis of clinical practice, is
presented as a mechanism that can counteract therapeutic persistence by promoting
empathetic communication and respect for patient dignity [26].
3.2. Degree of integration of palliative care in the ICU and its relationship to decision-making
The integration of palliative care into ICUs continues to be insufficient and uneven
in Latin America. While countries such as Brazil and Chile have developed institutional
initiatives that show a positive impact, in other cases, the lack of regulatory frameworks
and structured programs is a significant barrier [2, 4, 5, 8, 9, 15, 16, 27, 28, 29].
When compared with other regions, it is evident that even in consolidated health systems,
difficulties in integrating palliative programs early within critical care units persist,
which results in organizational barriers and cultural resistance [30]. Interprofessional studies demonstrate that factors such as team coordination and
ongoing education are key determinants in the quality of end-of-life decisions [31].
Likewise, humanization strategies applied in pediatric ICUs confirm that the incorporation
of palliative care not only improves communication with families but also strengthens
shared decision-making [32].
Clinical experiences in palliative extubation, in turn, show that this practice-in
addition to its technical demands-requires ethical and structural support for its
proper implementation [33].
All of this reinforces the need to consolidate regional policies that guarantee equitable
and effective access to palliative care in critical care settings.
3.3. Ethical and clinical competencies of healthcare professionals at the end of life
Significant deficiencies were identified in the ethical, clinical, and communication
training of healthcare personnel, which limits their ability to handle end-of-life
situations at the ICU. Among the most frequent challenges, there are limited experience
with the application of advanced directives, lack of training in the adjustment of
therapeutic effort, and fear of moral deliberation [17-20, 23-26, 34, 35].
Moreover, it is necessary to strengthen empathetic communication, assertiveness, and
interdisciplinary teamwork skills-areas that have been highlighted as essential to
ensure humanized, person-centered care [27, 34, 36]. Recent studies show that deficits in bioethics and palliative care training in
undergraduate and postgraduate programs limit professionals’ ability to make decisions
based on values and clinical evidence [37, 38].
Systematic reviews confirm that the implementation processes of palliative care in
the ICU must include institutional protocols and training programs that strengthen
clinical ethics and reduce variability in practice [30, 31, 39].
Literature also notes that clinical experiences in terminal weaning and extubation
at ICUs in Europe and North America reinforce the importance of ethical and communication
training as key elements in providing support to families [40, 41].
Taken together, the results show that therapeutic obstinacy in South American ICUs
stems from both structural and cultural factors, while the limited integration of
palliative care and the training gap in ethical-clinical competencies perpetuate this
phenomenon.
This analysis reaffirms the need to reform critical care models towards approaches
centered on dignity, ethical reflection, and the early integration of palliative care.
Table 1 presents the characteristics of the 30 studies sourced from five international and
regional databases.
Table 1
Description of the main characteristics and results of the studies
|
Specific objective
|
Relevant findings
|
References
|
|
1. Factors that favor the persistence of non-beneficial interventions in the ICU.
|
Absence of protocols, fear of legal repercussions, family pressure, and biomedical
hegemony make it difficult to recognize therapeutic futility and favor clinical obstinacy.
|
[1, 3, 4, 6, 7, 11-14, 21]
|
|
2. Degree of palliative care integration in the ICU and its relationship with decision-making.
|
Integration of palliative care in the ICU is low and uneven across the region; although
there are successful experiences, regulatory gaps and institutional and cultural barriers
that limit its consolidation persist.
|
[2, 4, 5, 8, 9, 15, 16, 27, 28, 29]
|
|
3. Ethical and clinical competencies of healthcare professionals at the end of life.
|
There are evident gaps in bioethics training, clinical communication, and the application
of AET, which hinders shared and ethically grounded decision-making at the end of
life.
|
[17-20, 23-26, 34, 35]
|
4. Discussion
Our findings suggest that the persistence of non-beneficial interventions in South
American ICUs is due to a complex interplay of structural, cultural, and educational
factors. This scenario not only reflects shortcomings in protocols and clinical guidelines,
but also a biomedical approach focused on prolonging life that hinders the recognition
of therapeutic futility.
This panorama partially coincides with what has been described in Europe and North
America, where ethical tensions have also been documented, but the implementation
of standardized protocols, robust regulatory frameworks, and training programs has
reduced variability and promoted AET practices [42, 43].
4.1 What do these findings mean in the South American context?
Results confirm that therapeutic obstinacy in South America is sustained by the absence
of institutional guidelines, fear of legal consequences, and family pressure. This
leads to fragmented decisions that are often far from therapeutic proportionality.
From a bioethical perspective, this phenomenon reveals a tension between the principles
of beneficence and non-maleficence, in which the continuation of invasive treatments
can increase suffering without delivering real benefit [44].
In addition, the predominantly curative medical culture delays the recognition of
the terminal nature of illness and limits the implementation of advanced care plans.
Studies in long-term care settings have shown that decision planning, including advanced
directives and early conversations, reduces family anxiety and enables choices consistent
with the patient's values [45].
In this scenario, therapeutic obstinacy is upheld by the absence of institutional
protocols, fear of legal repercussions, family pressure, and a biomedical culture
centered on curing. This shows that the bioethical debate has not yet translated into
clear policies or sufficient clinical training, resulting in fragmented decisions
that are often far from therapeutic proportionality and patient dignity.
4.2 How does this compare to international experiences?
In Europe, the application of the European Society of Intensive Care Medicine's guidelines
proposes clear algorithms for assessing futility, withdrawing life support, and ensuring
structured communication with family. Those tools could be adapted to South American
health systems to reduce clinical variability [40].
Meanwhile, in North America, recommendations of the American College of Critical Care
Medicine emphasize shared decision-making and comprehensive family support. Such practices
could be replicated in our region through training in clinical communication and psychosocial
support [38].
4.3 Response to the review objectives
Findings address the first specific objective of this research by confirming that
the persistence of non-beneficial interventions is based on the lack of protocols,
dominance of the curative culture, and legal fears, which perpetuate therapeutic obstinacy.
Regarding the second objective, there is evidence of low integration of palliative
care into ICUs. Isolated experiences in some countries highlight the need for mandatorily
incorporated palliative programs from the moment critically ill patients are admitted.
Finally, regarding the third objective, the review shows a training gap in bioethics,
communication, and clinical skills for end-of-life management. It confirms that not
strengthening these areas will make it difficult to systematically implement therapeutic
adjustments [46, 47].
4.4 Implications for clinical practice and health policy
These findings have direct implications for clinical practice: there is an urgent
need to implement standardized protocols for limiting therapeutic effort, structured
communication plans, and continuous education programs in bioethics and palliative
care.
At the public policy level, PAHO and WHO recommend integrating palliative care as
an essential part of universal health coverage; therefore, ensuring its availability
at all levels of care including ICUs [2, 5]. In the region, these recommendations could be turned into regulations requiring
the interdisciplinary and documented assessment of therapeutic proportionality, protecting
both patients and healthcare teams.
4.5 Knowledge gaps and future research lines
The review shows uneven scientific production in South America that limits the generalization
of findings. Multicenter studies are needed to assess the impact of early palliative
care integration programs on clinical indicators, family satisfaction, and staff well-being.
It is also recommended to investigate educational models to strengthen ethical and
communication skills in undergraduate and graduate programs in Medicine and Nursing.
Experiences such as reviews on palliative extubation in pediatric settings demonstrate
the importance of protocols that include emotional support for families and healthcare
teams [48, 49].
4.6 Strengths and limitations
One of the strengths of this work is the inclusion of recent and diverse literature,
which allowed for a contextualized and up-to-date analysis of the phenomenon in South
America. Additionally, the use of rigorous evaluation tools (PRISMA, ENTREQ, CASP)
[50] contributed to methodological robustness. However, the uneven availability of publications
in some countries may have introduced a geographic bias and limited the generalizability
of the findings.
Likewise, the methodological heterogeneity of the included studies poses a challenge
for the direct comparison of results.
4.7 Key message
The early and systematic integration of palliative care in the ICU-along with AET
protocols and ethical training for teams-is essential to reduce therapeutic obstinacy
and ensure patient-centered care focused on dignity and family involvement. South
America has the opportunity to adapt successful international models and turn them
into public policies that transform critical care into a more ethical, humane, and
sustainable practice.
5. Conclusions
The persistence of non-beneficial therapeutic interventions in palliative patients
assisted in South American ICUs reflects structural, educational, and cultural limitations
that hinder care centered on patient dignity. The integration of palliative care in
critical contexts is not only possible but necessary to guarantee more ethical, humane,
and sustainable medicine.
End-of-life decision-making must be based on bioethical principles, interdisciplinary
dialogue, and respect for patient values. In the long term, strengthening public policies,
institutional protocols, and professional training will be key to reducing therapeutic
relentlessness and improving the quality of care at ICUs in the region.
1. Introducción
En las últimas décadas, los avances tecnológicos en medicina crítica han posibilitado
prolongar la vida de pacientes con pronósticos que previamente eran considerados incompatibles
con la supervivencia. Sin embargo, estos avances también han planteado dilemas éticos
complejos, especialmente en relación con el uso de intervenciones médicas que, en
contextos de enfermedad avanzada o terminal, pueden ser consideradas fútiles o desproporcionadas.
Estas prácticas, conocidas como intervenciones terapéuticas no beneficiosas, no ofrecen
una mejora significativa en el pronóstico ni en la calidad de vida del paciente, lo
que plantea conflictos con los principios de autonomía, beneficencia, no maleficencia
y justicia [1].
En este contexto, los cuidados paliativos emergen como una respuesta ética, humanista
y científica. De acuerdo con la Organización Mundial de la Salud (OMS), este enfoque
se orienta a aliviar el sufrimiento y mejorar la calidad de vida de los pacientes
con enfermedades incurables o en fase terminal, así como las de sus familias [2]. Pese a esto, en las unidades de cuidados intensivos (UCI) de Sudamérica persiste
una tensión constante entre el uso de todos los recursos tecnológicos disponibles
y la necesidad de garantizar los principios de proporcionalidad terapéutica y dignidad
humana, lo que genera dilemas éticos y desafíos en la práctica asistencial [3, 4].
A pesar de su reconocimiento internacional como un componente esencial de la atención
sanitaria, la integración de los cuidados paliativos en las UCI de la región continúa
siendo escasa y desigual. Informes recientes de la Organización Panamericana de la
Salud (OPS) y diversos estudios regionales muestran que factores institucionales,
culturales y formativos dificultan la adopción de prácticas que prioricen el bienestar
integral del paciente en el final de la vida [5-9]. Además, los profesionales de la salud enfrentan incertidumbre clínica, presiones
familiares, temor a litigios y un enfoque curativo hegemónico, lo que limita la implementación
de decisiones compartidas y éticamente justificadas en contextos críticos [10-12].
La evidencia señala que la formación en ética clínica y la aplicación de estrategias
como la adecuación del esfuerzo terapéutico (AET) se constituyen como herramientas
fundamentales para prevenir el encarnizamiento terapéutico en contextos de cuidados
críticos [13, 14]. No obstante, aún se requiere mayor comprensión acerca de cómo estas estrategias
se implementan en la práctica cotidiana, especialmente en hospitales públicos y en
pacientes oncológicos o con mal pronóstico vital, casos en los que las decisiones
éticas suelen ser más complejas y se ven condicionadas por limitaciones estructurales
y culturales.
Ante esta problemática, el presente estudio se justifica por la necesidad de comprender
y reflexionar sobre las intervenciones terapéuticas no beneficiosas en pacientes paliativos
atendidos en UCI de Sudamérica. Estas prácticas no solo comprometen la calidad asistencial,
sino que entran en conflicto con principios fundamentales de la bioética y con el
reconocimiento de los cuidados paliativos como un derecho humano [15].
Igualmente, la incorporación limitada de este tipo de cuidados en los entornos críticos
de la región refleja una brecha de conocimiento y acción que, según las recomendaciones
internacionales, debe ser atendida mediante guías de implementación adaptadas al contexto
local [16].
Sumado a lo anterior, resulta indispensable promover procesos de atención centrados
en el paciente y su familia, sustentados en la ética del cuidado y la reflexión bioética
que integren el acompañamiento interdisciplinario y el respeto a la dignidad humana
[17, 18]. Para esto, la formación de los profesionales de la salud resulta clave para garantizar
decisiones clínicas fundamentadas en la evidencia y en los valores del paciente [19]. En este sentido, herramientas como la AET y las órdenes de no reanimar han sido
señaladas como recursos éticamente necesarios para enfrentar los dilemas al final
de la vida [20].
El objetivo de esta revisión es analizar la literatura científica reciente sobre el
abordaje de los cuidados paliativos y las intervenciones terapéuticas no beneficiosas
en unidades de cuidados intensivos de Sudamérica, identificando los factores que favorecen
la persistencia de dichas intervenciones en pacientes paliativos, explorando el grado
de integración de los cuidados paliativos en las UCI y su relación con la toma de
decisiones clínicas, y examinando las competencias éticas y clínicas de los profesionales
de salud frente al final de la vida en entornos críticos.
2. Metodología
2.1 Tipo de estudio
Se llevó a cabo una revisión de la literatura con un enfoque cualitativo.
2.2 Estrategia de búsqueda y selección de estudios
La búsqueda bibliográfica se realizó en las bases de datos PubMed, SciELO, Redalyc,
Dialnet y Google Scholar.
La estrategia de búsqueda se centró en combinar los descriptores DeCS/MeSH “cuidados
paliativos”, “unidades de cuidados intensivos”, “adecuación del esfuerzo terapéutico”,
“intervenciones terapéuticas no beneficiosas” y “Sudamérica”, con los operadores booleanos
AND y OR.
2.3 Criterios de inclusión
-
Artículos científicos arbitrados publicados en los últimos cinco años.
-
Artículos originales y artículos relevantes al objetivo de la investigación.
-
Literatura en idioma español e inglés.
2.4 Criterios de exclusión
-
Tesis, trabajos no arbitrados o ensayos sin metodología clara.
-
Artículos centrados en cuidados paliativos domiciliarios o extrahospitalarios.
-
Publicaciones anteriores al año 2021.
2.5 Proceso de selección
Inicialmente, se identificaron 94 artículos potencialmente relevantes. Tras aplicar
los criterios de inclusión y exclusión se seleccionaron 30 que cumplían con la pertinencia
temática requerida y que se muestra en un diagrama de flujo PRISMA.
2.6 Instrumentos de evaluación de calidad metodológica
Para asegurar la transparencia y el rigor de la revisión, se aplicaron los siguientes
instrumentos:
-
Checklist Enhancing Transparency in Reporting the Synthesis of Qualitative Research
(ENTREQ): cumplimiento de 18 de los 21 ítems.
-
Checklist PRISMA 2020: cumplimiento de 26 de los 27 ítems. No se realizó registro
en el International Prospective Register of Systematic Reviews (PROSPERO).
-
Critical Appraisal Skills Programme (CASP): aplicación de los diez criterios para
estudios cualitativos, con cumplimiento de nueve de ellos. Se identificó como principal
limitación la escasa reflexividad explícita de los investigadores en algunos estudios.
2.7 Procedimientos de análisis
Los estudios incluidos fueron sometidos a una evaluación crítica individual mediante
la versión cualitativa del CASP, considerando diseño, método de recolección de datos,
claridad en la presentación de resultados, implicaciones clínicas y rigor metodológico.
Estas herramientas y procedimientos aseguraron la reproducibilidad, transparencia
y validez metodológica del presente estudio, aportando una base sólida para el análisis
y la formulación de recomendaciones clínicas y éticas.
3. Resultados
Inicialmente, se identificaron 94 registros en las bases de datos SciELO, Redalyc,
PubMed, Dialnet y Google Scholar. Tras la eliminación de 16 duplicados, se revisaron
78 títulos y resúmenes, de los cuales 40 fueron considerados potencialmente relevantes
para lectura a texto completo. Finalmente, 30 estudios cumplieron con los criterios
de inclusión y fueron incorporados en la síntesis cualitativa de la revisión (Figura 1).
Figura 1
Diagrama de flujo de la selección de los artículos, según el modelo PRISMA
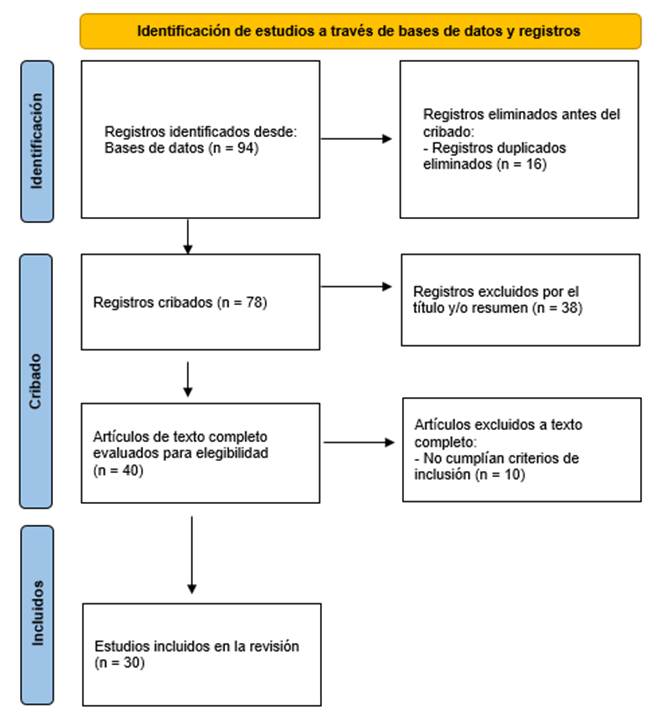
Fuente: elaboración propia con base en el flujograma PRISMA 2020.
Los hallazgos se organizaron en torno a los tres objetivos específicos definidos en
la revisión, como se expondrá a continuación.
3.1. Factores que favorecen la persistencia de intervenciones no beneficiosas en UCI
Los hallazgos confirman que la persistencia de intervenciones no beneficiosas en pacientes
críticos está relacionada con múltiples factores de orden estructural, cultural y
legal. Entre los más destacados se encuentran la ausencia de protocolos institucionales,
la presión familiar y el temor a repercusiones jurídicas, lo que conduce a prolongar
la vida con tratamientos invasivos en escenarios sin posibilidades de recuperación
[1, 3, 6, 7, 11-14, 21].
Complementariamente, otros estudios han subrayado el impacto de la digitalización
de la medicina y la creciente tecnificación del cuidado crítico en los que la dependencia
de dispositivos médicos refuerza prácticas de obstinación terapéutica [22]. A su vez, investigaciones recientes evidencian que la cultura biomédica en América
Latina, fuertemente orientada a la curación, dificulta reconocer oportunamente la
futilidad terapéutica y limita el desarrollo de espacios de deliberación ética [23-25].
La humanización del cuidado, entendida como eje fundamental en la práctica clínica,
se plantea como un mecanismo que puede contrarrestar el encarnizamiento terapéutico
al favorecer la comunicación empática y el respeto por la dignidad del paciente [26].
3.2. Grado de integración de cuidados paliativos en UCI y su relación con la toma
de decisiones
La integración de cuidados paliativos en UCI continúa siendo insuficiente y heterogénea
en América Latina. Mientras países como Brasil y Chile han desarrollado experiencias
institucionales que muestran impacto positivo; en otros casos, la falta de marcos
normativos y programas estructurados representa una barrera significativa [2, 4, 5, 8, 9, 15, 16, 27, 28, 29].
Al comparar con otras regiones se observa que, incluso en sistemas de salud consolidados,
persisten dificultades para integrar programas paliativos de manera temprana en unidades
críticas, lo que se traduce en barreras organizativas y resistencias culturales [30]. Estudios interprofesionales demuestran que factores como la coordinación entre
equipos y la educación continua son determinantes en la calidad de las decisiones
al final de la vida [31].
De la misma forma, estrategias de humanización aplicadas en UCI pediátricas confirman
que la incorporación de cuidados paliativos no solo mejora la comunicación con las
familias, sino que fortalece la toma de decisiones compartidas [32].
Por su parte, experiencias clínicas en extubación paliativa evidencian que esta práctica,
además de su carga técnica, requiere soporte ético y estructural para su correcta
implementación [33].
Todo ello refuerza la necesidad de consolidar políticas regionales que garanticen
el acceso equitativo y efectivo a los cuidados paliativos en entornos críticos.
3.3. Competencias éticas y clínicas de los profesionales de salud frente al final
de la vida
Se identificaron deficiencias relevantes en la formación ética, clínica y comunicacional
del personal sanitario, lo que limita su capacidad para enfrentar situaciones de final
de vida en UCI. Entre las dificultades más frecuentes se destacan la escasa experiencia
en la aplicación de voluntades anticipadas, la falta de entrenamiento en adecuación
del esfuerzo terapéutico y el temor a la deliberación moral [17-20, 23-26, 34, 35].
A este panorama, se suma la necesidad de fortalecer competencias en comunicación empática,
asertividad y trabajo interdisciplinario, aspectos que han sido señalados como esenciales
para garantizar un cuidado humanizado y centrado en la persona [27, 34, 36]. Estudios recientes demuestran que el déficit de formación en bioética y cuidados
paliativos en los programas de pregrado y posgrado limita la capacidad de los profesionales
para tomar decisiones fundamentadas en valores y evidencia clínica [37, 38].
Revisiones sistemáticas confirman que los procesos de implementación de cuidados paliativos
en UCI deben incluir protocolos institucionales y programas formativos que fortalezcan
la ética clínica y reduzcan la variabilidad en la práctica [30, 31, 39].
La literatura también destaca que las experiencias clínicas en destete terminal y
extubación en UCI de Europa y Norteamérica refuerzan la importancia de la capacitación
ética y comunicacional como elementos clave para el acompañamiento familiar [40, 41].
En conjunto, los resultados muestran que la obstinación terapéutica en UCI de Sudamérica
responde tanto a factores estructurales como culturales, mientras que la escasa integración
de cuidados paliativos y la brecha formativa en competencias ético-clínicas perpetúan
este fenómeno.
Este análisis reafirma la necesidad de reformar los modelos de atención crítica hacia
enfoques centrados en la dignidad, la reflexión ética y la integración temprana de
cuidados paliativos.
La Tabla 1 recoge las características de los 30 estudios provenientes de cinco bases de datos
internacionales y regionales.
Tabla 1
Descripción de las principales características y resultados de los estudios
|
Objetivo específico
|
Hallazgos relevantes
|
Referencias
|
|
1. Factores que favorecen la persistencia de intervenciones no beneficiosas en UCI
|
La ausencia de protocolos, el temor a repercusiones legales, la presión familiar y
la hegemonía biomédica, dificultan reconocer la futilidad terapéutica y favorecen
la obstinación clínica.
|
[1, 3, 4, 6, 7, 11-14, 21]
|
|
2. Grado de integración de cuidados paliativos en UCI y su relación con la toma de
decisiones
|
La integración de cuidados paliativos en UCI es baja y desigual en la región; aunque
existen experiencias exitosas, persisten vacíos normativos, barreras institucionales
y culturales que limitan su consolidación.
|
[2, 4, 5, 8, 9, 15, 16, 27, 28, 29]
|
|
3. Competencias éticas y clínicas de los profesionales de salud frente al final de
la vida
|
Se evidencian carencias en formación bioética, comunicación clínica y aplicación de
AET, lo que dificulta decisiones compartidas y éticamente fundamentadas en el final
de la vida.
|
[17-20, 23-26, 34, 35]
|
4. Discusión
Nuestros hallazgos sugieren que la persistencia de intervenciones no beneficiosas
en UCI sudamericanas responde a un entramado de factores estructurales, culturales
y formativos. Este escenario no solo refleja carencias en protocolos y guías clínicas,
sino un enfoque biomédico centrado en la prolongación de la vida que dificulta reconocer
la futilidad terapéutica.
Este panorama coincide parcialmente con lo descrito en Europa y Norteamérica donde
también se han documentado tensiones éticas, pero la implementación de protocolos
estandarizados, marcos regulatorios robustos y programas de formación ha reducido
la variabilidad y favorecido prácticas de AET [42, 43].
4.1 ¿Qué significan los hallazgos en el contexto sudamericano?
Los resultados confirman que la obstinación terapéutica en Sudamérica se sostiene
por la ausencia de guías institucionales, el temor a consecuencias legales y la presión
familiar, lo que deriva en decisiones fragmentadas y frecuentemente alejadas de la
proporcionalidad terapéutica. Desde una perspectiva bioética, este fenómeno revela
una tensión entre los principios de beneficencia y no maleficencia en la que la continuidad
de tratamientos invasivos puede incrementar el sufrimiento sin aportar beneficios
reales [44].
De igual forma, la cultura médica predominantemente curativa retrasa el reconocimiento
del carácter terminal de la enfermedad y limita la implementación de planes de cuidado
anticipado. Estudios en contextos de cuidados de larga estancia han demostrado que
la planificación anticipada de decisiones incluyendo voluntades anticipadas y conversaciones
tempranas reduce la ansiedad familiar y facilita elecciones coherentes con los valores
del paciente [45].
En este escenario, la obstinación terapéutica se sostiene por la ausencia de protocolos
institucionales, el temor a repercusiones legales, la presión familiar y una cultura
biomédica centrada en la curación. Esto muestra que el debate bioético no se ha traducido
aún en políticas claras ni en formación clínica suficiente, lo que genera decisiones
fragmentadas y muchas veces alejadas de la proporcionalidad terapéutica y la dignidad
del paciente.
4.2 ¿Cómo se comparan con experiencias internacionales?
En Europa, la aplicación de guías de la Sociedad Europea de Cuidados Intensivos propone
algoritmos claros para evaluar futilidad, retirar soporte vital y garantizar comunicación
estructurada con la familia, herramientas que podrían adaptarse a los sistemas de
salud sudamericanos para reducir la variabilidad clínica [40].
Por su parte, en Norteamérica, las recomendaciones del American College of Critical
Care Medicine enfatizan en la toma de decisiones compartidas y el acompañamiento integral
de la familia, prácticas replicables en nuestra región mediante formación en comunicación
clínica y soporte psicosocial [38].
4.3 Respuesta a los objetivos de la revisión
Los hallazgos dan respuesta al primer objetivo específico de esta investigación al
confirmar que la persistencia de intervenciones no beneficiosas se sustenta en la
falta de protocolos, la hegemonía de la cultura curativa y el temor legal, lo que
perpetúa la obstinación terapéutica.
Respecto al segundo objetivo, se evidencia una baja integración de cuidados paliativos
en UCI, con experiencias aisladas en algunos países, lo que sugiere la necesidad de
incorporar de forma obligatoria programas paliativos desde el ingreso de pacientes
críticos.
Finalmente, en relación con el tercer objetivo, la revisión muestra una brecha formativa
en bioética, comunicación y competencias clínicas para el manejo del final de la vida,
confirmando que sin un fortalecimiento de estas áreas será difícil implementar adecuaciones
terapéuticas de manera sistemática [46, 47].
4.4 Implicaciones para la práctica clínica y la política de salud
Estos hallazgos tienen implicaciones directas para la práctica clínica: urge implementar
protocolos estandarizados de limitación del esfuerzo terapéutico, planes de comunicación
estructurados y programas de educación continua en bioética y cuidados paliativos.
A nivel de políticas públicas, la OPS y la OMS recomiendan integrar los cuidados paliativos
como parte esencial de la cobertura universal de salud, lo que implica garantizar
su disponibilidad en todos los niveles de atención, incluidas las UCI [2, 5]. En la región, estas recomendaciones podrían traducirse en normativas que obliguen
a evaluar la proporcionalidad terapéutica de manera interdisciplinaria y documentada,
protegiendo tanto a pacientes como a equipos de salud.
4.5 Vacíos de conocimiento y líneas de investigación futuras
La revisión muestra una producción científica desigual en Sudamérica, lo que limita
la generalización de los hallazgos. Se requieren estudios multicéntricos que evalúen
el impacto de programas de integración temprana de cuidados paliativos en indicadores
clínicos, satisfacción familiar y bienestar del personal.
Asimismo, se recomienda investigar modelos pedagógicos para fortalecer competencias
éticas y comunicacionales en los pregrados y posgrados en Medicina y Enfermería. Experiencias
como las revisiones sobre extubación paliativa en entornos pediátricos demuestran
la importancia de protocolos que incluyan soporte emocional para las familias y los
equipos de salud [48, 49].
4.6 Fortalezas y limitaciones
Una fortaleza del presente trabajo es la inclusión de literatura reciente y diversa,
lo que permitió un análisis contextualizado y actualizado del fenómeno en Sudamérica.
A su vez, el uso de herramientas de evaluación rigurosas (PRISMA, ENTREQ, CASP) [50] aportó solidez metodológica. Sin embargo, la disponibilidad desigual de publicaciones
en algunos países pudo haber introducido un sesgo geográfico y limitar la generalización
de los hallazgos.
Igualmente, la heterogeneidad metodológica de los estudios incluidos representa un
desafío para la comparación directa de resultados.
4.7 Mensaje clave
La integración temprana y sistemática de los cuidados paliativos en UCI, acompañada
de protocolos de AET y formación ética de los equipos, es indispensable para reducir
la obstinación terapéutica y garantizar una atención centrada en la dignidad del paciente
y el acompañamiento familiar. La región sudamericana tiene la oportunidad de adaptar
modelos internacionales exitosos y convertirlos en políticas públicas que transformen
la atención crítica en una práctica más ética, humana y sostenible.
5. Conclusiones
La persistencia de intervenciones terapéuticas no beneficiosas en pacientes paliativos
asistidos en UCI sudamericanas refleja limitaciones estructurales, formativas y culturales
que impiden una atención centrada en la dignidad del paciente. La integración de cuidados
paliativos en contextos críticos no solo es posible, sino necesaria para garantizar
una medicina más ética, humana y sostenible.
La toma de decisiones en el fin de la vida debe fundamentarse en principios bioéticos,
diálogo interdisciplinario y respeto por los valores del paciente. A largo plazo,
el fortalecimiento de políticas públicas, protocolos institucionales y formación profesional
será clave para reducir el encarnizamiento y mejorar la calidad de los cuidados en
las UCI de la región.